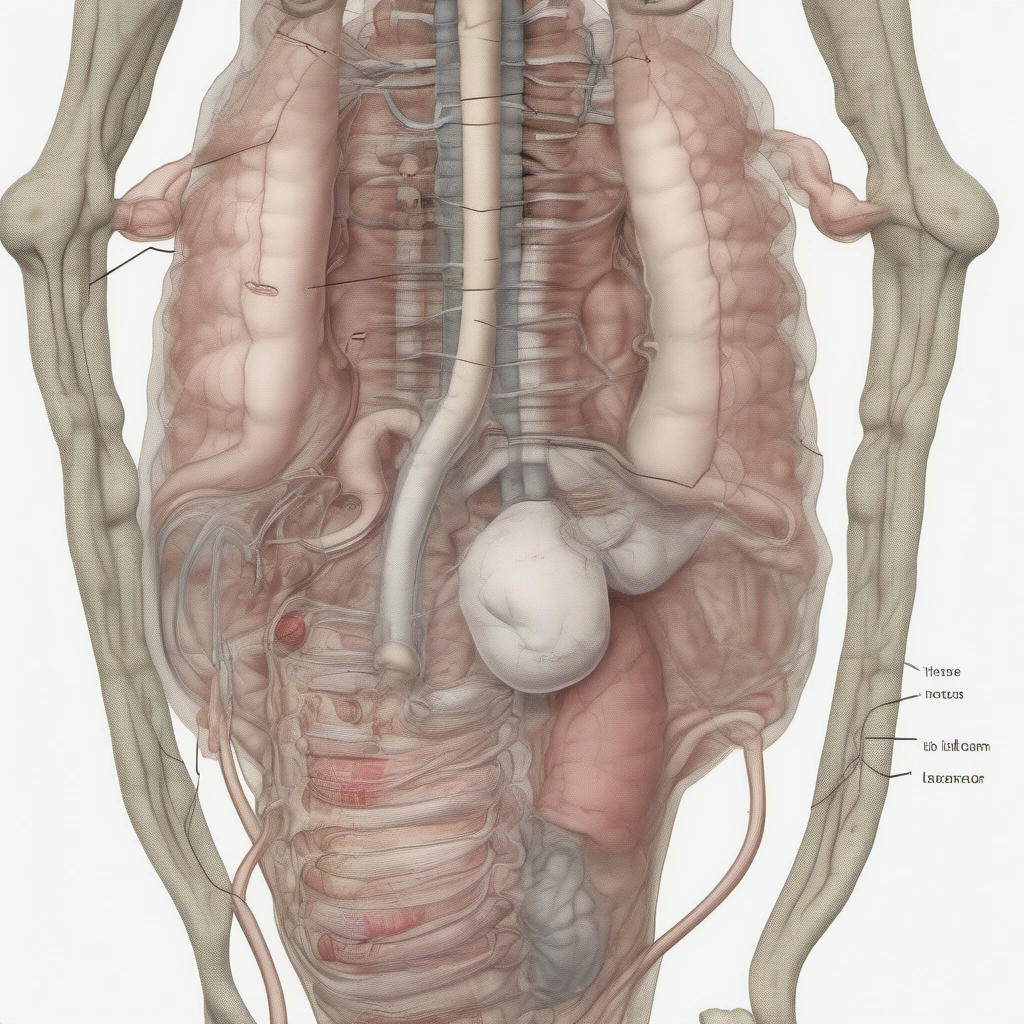
Anal prolapse is a condition where the rectum or a portion of the large intestine slips or slides out of place and through the anal opening. This can be a painful and uncomfortable condition that should be addressed promptly to prevent further complications. The following guide offers a detailed exploration of anal prolapse, including ways to recognize it, causes, and associated medical considerations that must be taken into account.
Recognizing Anal Prolapse
Noticeable Bulge: The most common sign of anal prolapse is a visible, circular, or tube-like bulge or mass protruding from the anus. It may be soft and spongy to the touch.
Discomfort or Pain: Individuals with anal prolapse may feel a sense of fullness in the rectum, or experience varying degrees of pain and discomfort during bowel movements or when sitting for long periods. The prolapsed tissue can cause pressure and irritation, particularly when straining during defecation.
Excessive Mucus or Bleeding: In some cases, individuals with anal prolapse may notice excessive mucus seeping from the anus, or spot blood on the toilet paper or stool after a bowel movement.
Causes of Anal Prolapse
Chronic Constipation: Constipation can cause prolonged straining during bowel movements, putting pressure on the rectum and loosening the supporting connective tissues, eventually leading to a prolapse.
Inflammatory Bowel Disease (IBD): Conditions such as Crohn's disease and ulcerative colitis can cause inflammation and scarring, which may weaken the tissues supporting the rectum, increasing the risk of prolapse.
Pregnancy and Childbirth: The pressure exerted on the pelvic floor during pregnancy and the strain during delivery can weaken the muscles and tissues in the rectal area, potentially causing prolapse or exacerbating an existing one.
Aging and Weakened Pelvic Floor: As we age, our muscles, including the pelvic floor muscles, weaken. This weakening, combined with factors like a history of chronic constipation or a weakened pelvic floor due to childbirth, can increase the risk of prolapse.
Maintain Healthy Bowel Habits: Eating a diet rich in fiber, staying hydrated, and avoiding straining during bowel movements can help prevent constipation, which is a leading contributor to anal prolapse.
Pelvic Floor Exercises: Practicing Kegel exercises to strengthen the pelvic floor muscles can help protect against prolapse.
Attending Regular Checkups: Getting routine physical examinations that include rectal checks can catch any early signs of prolapse.
Prompt Medical Attention: Seeking timely medical attention when symptoms of prolapse appear is crucial to prevent complications and undergo appropriate treatment.
Anal prolapse is a condition that should not be taken lightly. It can cause discomfort, pain, and if left unaddressed, can lead to more severe complications. By being aware of the signs and symptoms, seeking prompt medical attention when needed, and following preventive measures, individuals can manage this condition effectively and maintain a good quality of life despite having anal prolapse.